Configuring Insurance Plans
If you plan to print or send electronic claims, you will need to configure the Insurance Plans before assigning them to the patient.
Note: This page includes generic Add and Edit Functionality
Add New: opens a new record at the bottom of the window with all of the fields empty. Please carefully review the existing descriptions to see if one of them may work BEFORE adding a description to the system
Add as New: must be selected to save the information after completing the empty Add New screen. May be selected when an existing record is in focus and you wish to create a copy of that record instead of creating a new, blank record.
Save Modifications: must be selected when you have made changes to an existing record and you wish to save the changes.
Add a New Plan to System
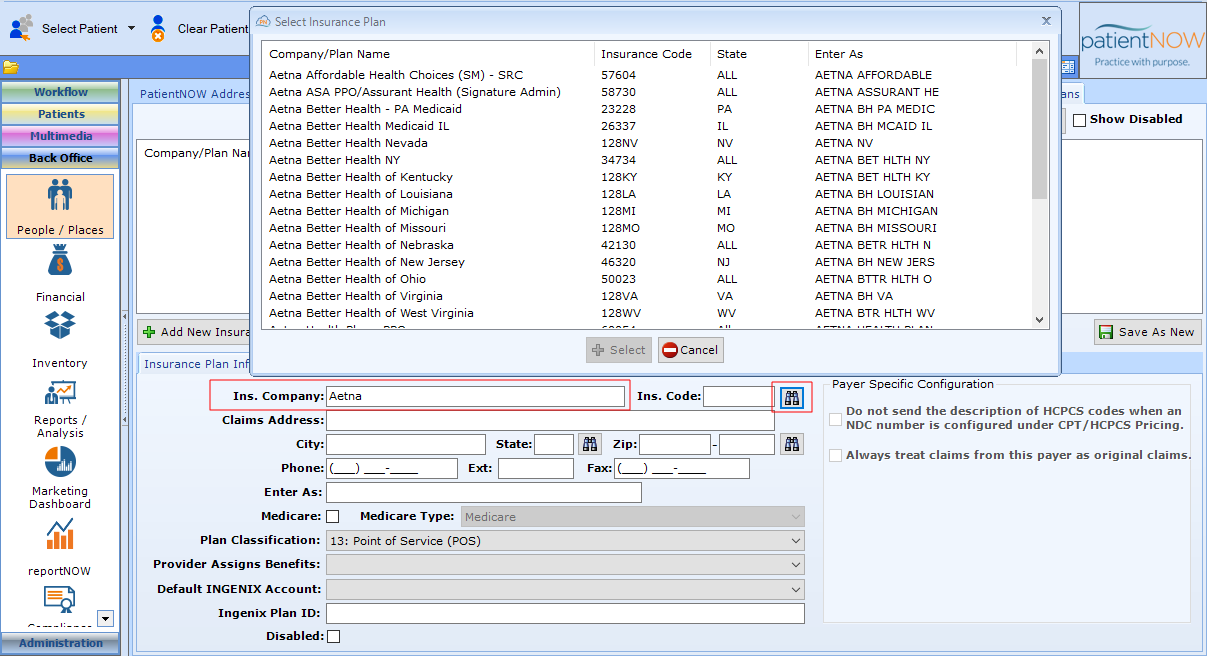
Navigate to Back Office | People / Places, Insurance Plans tab.
Select Add Insurance Plan and search for the plan you wish to add.
To search, enter a part of the insurance company name in the Ins. Company field and click the binoculars.
Select the correct plan. Note: if you have the patient's insurance card and you can find the edi #, you can also search by that number. Just leave the Ins. Company field blank and enter the # in the Ins. Code field.
Complete the remaining information. Some of the items are required and some are optional.
Required Items
- Ins. Company. Name of Company as found in search.
- Ins. Code. Automatically filled in when you search.
- If the plan is a Medicare plan (or Medicare Replacement), you must select
- the Medicare checkbox
- The Medicare Type (Medicare or RailRoad Medicare)
- Plan Classification; if you are not sure, use 13: Point of Service (POS) as a default.
- Provider Assigns Benefits. If you select C: Not Assigned, the reimbursement may be made to the patient, not to you.
- Ingenix Plan ID. MUST be exactly the same as the Ingenix Plan ID.
Optional Items
- Claims Address, City, State, Zip. Not required for electronic claims, but useful and required for printed claims or follow-up with the plan.
- Default Ingenix Account. If you need to use a specific Ingenix (Optum) account configured in Administration | Financial Admin, INGENIX Accounts tab, you may select that here.
- Payer Specific Configuration. Check the boxes if this payer:
- Does NOT want a description of medications; they just want the NDC Number.
- Does NOT accept Corrected Claims.
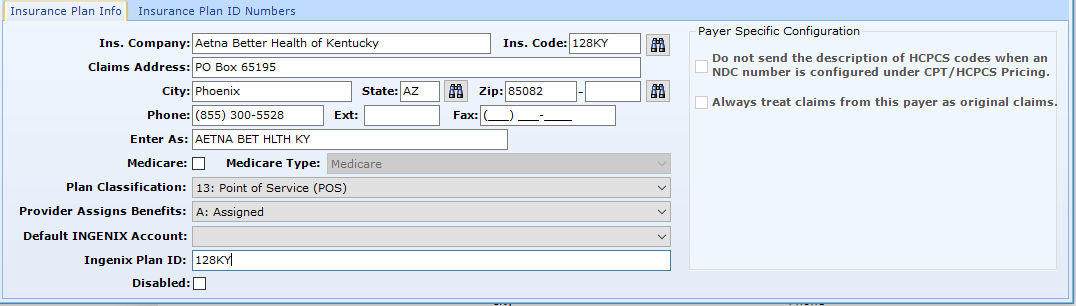
Select Add as New.
Insurance Plan ID Numbers
If the plan requires that you send the provider's number that is specific to that plan (in addition to the NPI), you may enter them.
Navigate to the Insurance Plan ID Number subtab.
Select Add and Complete the Information.
- Provider or Facility. If the number is specific to a provider, select that option. If the number is specific to a group or facility, select Facility.
- ID Type.
- ID Number.
Select OK.